The UK National Health Service (NHS) has a database containing 11 million patient records from 550 general practices (primary care) in the UK and studies have shown that this database is representative of the UK in general. As the UK healthcare system is not substantially different to other countries with a well-funded healthcare system, the data will be representative for these countries as well. All these data look back in time and will therefore only include wound care products that are well-integrated into standard practice. The data will not include MPPT (Amicapsil).
Dr. Julian Guest and colleagues have used this database to determine the success rate of wound care in the UK in the primary care sector. They asked what was the outcome for four different wound types within 12 months of first presentation to a general practice? The papers cover a great level of detail, but the most fundamental questions must be how many wounds heal and how long does it take?
| Table 1 | % healed | Time to healing (months) | Mean cost per patient (12 months) |
| Pressure ulcers | 50% | 5.4 | £8,720 |
| Diabetic foot ulcers | 35% | 4.4 | £7,800 |
| Venous leg ulcers | 53% | 3.0 | £7,600 |
| Surgical wounds | 83% | 4.0 | £7,300 |
Table 1 shows for 4 common wound types the percentage of wounds that healed, i.e. closed, within 12 months of first presentation; the time to healing for the wounds that did heal; and mean cost per patient for these 12 months. These data include all wounds of a specific type from the very minor to the very severe.
For ulcers, the table shows that only 50% or less heal within the first year. Surgical wounds have a higher probability of healing, but 17% remained unhealed. For the ulcers and surgical wounds that did heal, it took on average 4 months. The average costs were comparable across wound type and were around £7500 per wound.
| Table 2 | % healed | Time to healing (months) | Mean cost per patient (12 months) |
| Pressure ulcers | 14% | 7.7 | £10,906 |
| Diabetic foot ulcers | 16% | 6.1 | £11,585 |
| Venous leg ulcers | 25% | 4.9 | £12,893 |
| Surgical wounds | 85% | 6.5 | £8,742 |
Table 1 included all wounds, whereas Table 2 summarises the same data for patients with an infected wound who had received oral antibiotics and possibly wound dressings designed to remove the infection. For these infected wounds, the percentage of ulcers healing within the first 12 months was less than 20%, i.e. 4 out of 5 patients did not heal within 12 months. For surgical wounds, 85% heal, but 15% remain unhealed. The time to healing for the wounds and ulcers that do heal are around 6 months, i.e. half a year. The implications for patient quality-of-life are substantial, e.g. pressure ulcers often require bed-rest to heal, but 86% are still not closed after 1 year – and there is no guarantee that the ulcer will ever close. The average costs for these wounds over a 12-month-period was approximately £11,500 for ulcers and £8750 for surgical wounds.
The FDA in 2016 concluded that wound dressings with antibiotics and antimicrobials are ineffective in removing wound infections and in supporting healing. Furthermore, NICE in the UK in their guidance on pressure ulcers recommends that antibiotics, antiseptics and NPWT not be used routinely in the treatment of pressure ulcers due to lack of efficacy. The above data are fully in line with the conclusions reached by both the FDA and NICE. The tables also highlight the amount of resources that are used on treating these wounds and question why the healthcare systems are opposed to the introduction of new treatments, which act through different mechanisms, such as e.g. MPPT (Amicapsil).
An added complication for individuals with spinal cord injury (SCI), multiple sclerosis (MS) and diabetes, is that their immune system is compromised because of changes in their nervous system. The nervous system senses local injuries and infections through sensory fibers and it activates the immune system through the sympathetic nervous system. However, these systems are affected in SCI, MS and diabetes with the consequence that it is difficult for the body to detect the wound or an infection and to coordinate the healing of these wounds. Instead the wounds continue to deteriorate and cause secondary complications, e.g. bone infection, septicaemia and sinus tract formation. So, any person affected by one of these conditions should react immediately if they develop a wound because they can easily become life-threatening.
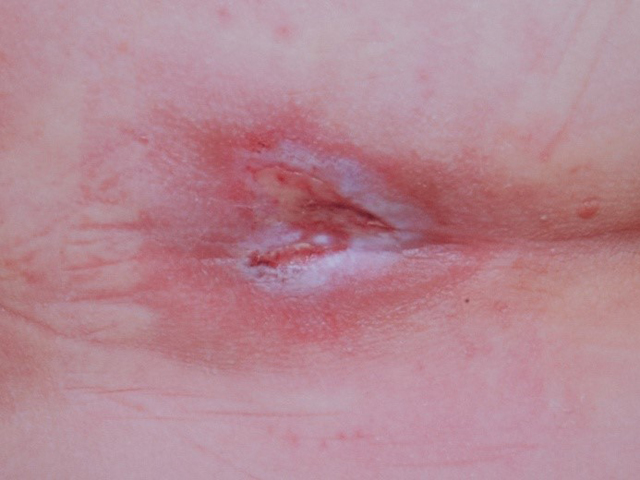
Examples of wounds treated with “standard-of-care” are shown below.
Examples of wounds deteriorating with standard-of-care treatment. Top row: daily wound wash with Prontosan followed by application of silver dressings; middle row: iodine treatment twice weekly – the wound appeared in May and treatment with iodine was started in June and was has already by August deteriorating; bottom row: long array of dressings and NPWT were tried, but unsuccessfully.
References
Guest JF, Fuller GW, Vowden P. Costs and outcomes in evaluating management of unhealed surgical wounds in the community in clinical practice in the UK: a cohort study. BMJ Open. 2018 Dec 14;8(12):e022591. doi: 10.1136/bmjopen-2018-022591.
Guest JF, Fuller GW, Vowden P, Vowden KR. Cohort study evaluating pressure ulcer management in clinical practice in the UK following initial presentation in the community: costs and outcomes. BMJ Open. 2018 Jul 25;8(7):e021769. doi: 10.1136/bmjopen-2018-021769.
Guest JF, Fuller GW, Vowden P. Diabetic foot ulcer management in clinical practice in the UK: costs and outcomes. Int Wound J. 2018 Feb;15(1):43-52. doi: 10.1111/iwj.12816.
Guest JF, Fuller GW, Vowden P. Venous leg ulcer management in clinical practice in the UK: costs and outcomes. Int Wound J. 2018 Feb;15(1):29-37. doi: 10.1111/iwj.12814.
Guest JF, Vowden K, Vowden P. The health economic burden that acute and chronic wounds impose on an average clinical commissioning group/health board in the UK. J Wound Care. 2017 Jun 2;26(6):292-303. doi: 10.12968/jowc.2017.26.6.292.
Guest JF, Ayoub N, McIlwraith T, Uchegbu I, Gerrish A, Weidlich D, Vowden K, Vowden P. Health economic burden that different wound types impose on the UK’s National Health Service. Int Wound J. 2017 Apr;14(2):322-330. doi: 10.1111/iwj.12603.