Amicapsil was used on this wound for 4 months from late June to mid-October and had been able to remove a wound infection and advance the healing of the wound. Please refer to the case report “35 year old infected necrotic abscess following radiation therapy”.
The case described below has been published: Sams-Dodd J and Sams-Dodd F. (2020) MPPT Promotes Wound Healing, Whereas PHMB Causes Tissue Degeneration: A Case Report. Wounds 32(3):E6–E10.
By mid October 2017, the progress had been impressive and the status of the wound was:
- The 20 cm deep sinus was cleared of slough and remaining clean
- The wound was practically cleared of necrotic tissue.
- The purple-red cellulitic wound edges had changed to healthy pink and were epithelialising.
- The undermining was reducing.
- The wound had reduced by 50% in volume and was still reducing via strong granulation.
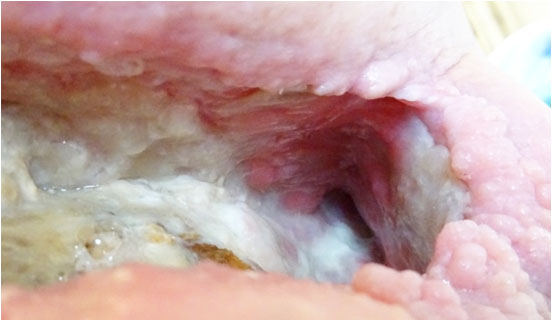
- The left half of the floor area of the wound was located on top of the osteomyelitic bone. This was clear of necrotic tissue whilst the white and structured fascia on top of the bone was preserved. The grey and brown protrusions through the fascia are deformations of the chronic osteomyelitic bone. Granulation had started to grow back over the bone particularly where the fascia was intact.

For reasons external to Amicapsil and the healing of the wound, the treatment protocol was changed from the use of Amicapsil (stopped 17 October 2017) into the use of PHMB (first application 20 October 2017). After 2 days with only absorbent dressing, the wound was applied every other day PHMB (0.1% PHMB aka Polihexanide; and betaine surfactant) combined with gelling fiber packing covered with an occlusive foam dressing.
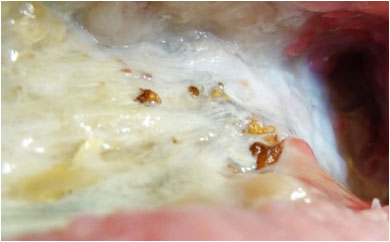
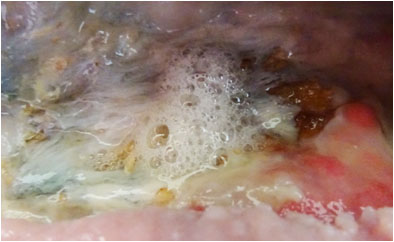
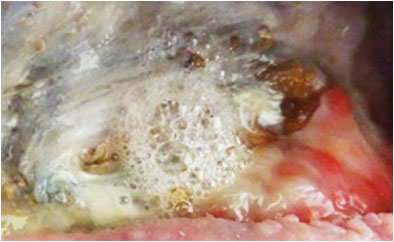
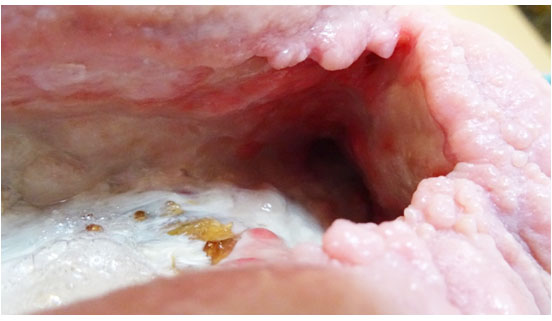
On Day 6 (Pict. 26 October 2017), froth appeared in one area of the exposed hip bone, indicative of gas produced by anaerobic bacteria entering the wound through holes in the underlying infected bone. This had not previously been seen and the holes had, most likely, formed in the bone since the start of PHMB application. The froth would increase in volume over the subsequent days and continued after PHMB was later stopped. Holes from the wound into the infected bone will increase the ease of access of toxins and pathogenic (disease causing) microbes into the wound.
Pictures above showing the development of froth formation.
Healthy granulation tissue is pink and, if it is actively granulating, it is covered with a new layer of shiny opaque white cells, i.e. the proliferation layer. As these cells mature and vascularisation is built up (angiogenesis), this gradually turns pink and is easily recognisable as granulation tissue. Vividly granulating tissue will, therefore; usually wear a constant white “cap” of new cells on top of the maturing layers underneath.
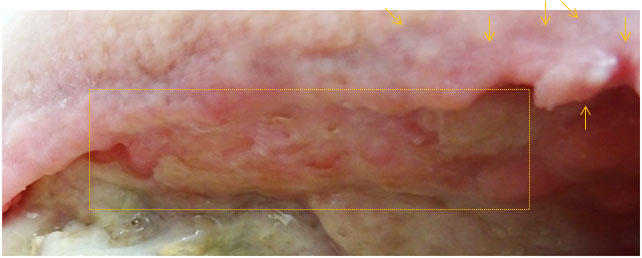
After start of application, the granulation tissue gradually began to lose its white proliferation layer which left the granulation increasingly red and irritated. Regression of the granulation tissue was observed.
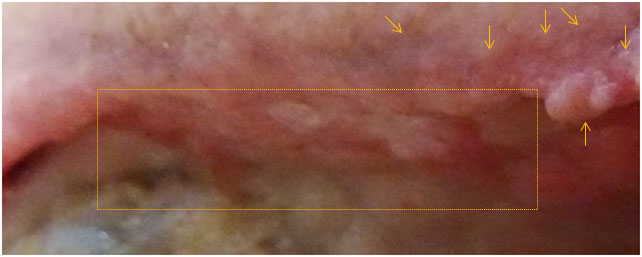
In areas that had already undergone strong build-up and maturation, the granulation buds lost their white cover, the areas flattened, no longer exposing bud-formation, and even regressed markedly. This is easily observed within the rectangles in the pictures below.
Pictures above showing changes to granulation and wound edges.
Furthermore, the wound edges changed from epithelialising whitish pink into a shrivelling red-to-purple appearance. The yellow arrows allow comparison of the same locations at the two time points in the picture above.
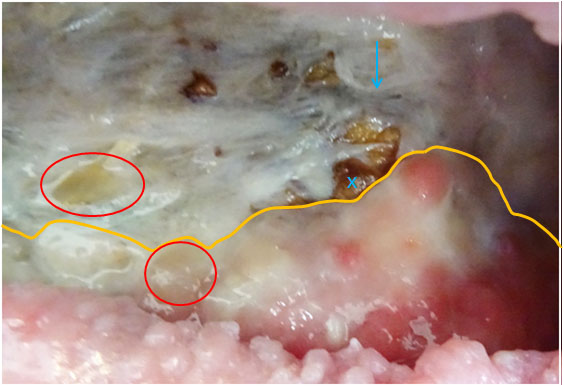
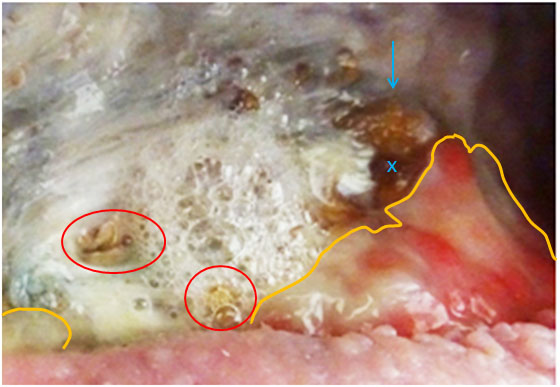
In areas where the granulation had started to move across the fascia covering the osteomyelitic bone, it would regress, as well. (In the pictures below, the yellow lines indicate the front edges of the granulation tissue).
Changes in the tissue, facia and bone across the exposed hip-bone in pictures above.
The fascia on top of the exposed hip bone regressed in certain places and lost its structured appearance. The changes to the fascia resulted in increased direct exposure of the underlying infected bone. An example of this is evident from the pictures above, where the blue arrows and crosses indicate the exact same spot. Likewise, it would also result in increased difficulty for granulation tissue to migrate across
Likewise, the red circles indicate the same positions in the two wounds, showing that PHMB removed the proliferating granulation in both spots exposing holes directly into the underlying bone. Direct communication, e.g. via perforations of the bone, would result in increased release of toxins and pathogens (that cause infection) into the wound.
Exudate and slough increased in volume and changed in colour from yellow into dark-brown to black as would be apparent on the packing and outer dressings.
After 10 days’ use of PHMB, an acute pain syndrome developed in the wound, where-after the use of PHMB was stopped.
All these changes were indicative of cytotoxic damage to the cells. As PHMB remains in the cells for several days, a 7 day wash-out period of PHMB was required. During this time, the effects initiated by PHMB continued. The patient returned to the use of Acapsil and over the following month the changes were gradually reversed and the strong healing process restored. The pictures below are from 4 days into the wash-out period and 2 months later and show considerable reduction in wound volume.
In summary
- Amicapsil was applied to the wound for 4 consecutive months – including directly on top of osteomyelitic bone – and strongly supported healing and caused no side effects.
- 10 days of PHMB application caused cell damage and regression of the healing process.
- Amicapsil reversed these effects and returned the wound to a quickly progression of healing, again with no side-effects.
The cytotoxic effects seen with the use of PHMB have also been identified in cell culture studies (Yabes et al. 2017) and in a recognised animal model of wound healing (Carroll and Ingram 2017; Carroll et al. 2017). See the section on Antiseptics.