












100% closure rate of pressure ulcers
Download Publication
Download Publication
Download Publication
NH ( patient)
NH ( patient)
NH ( patient)
Only natural ingredients
Only natural ingredients
Only natural ingredients
VH (patient)
VH (patient)
VH (patient)
Spinal cord injury, wounds and osteomyelitis
A spinal cord injury disrupts communication between the nervous system and the immune system. This means that the nervous system cannot activate the immune response if there is an injury or an infection and it cannot direct the immune cells to the location of the condition. The result is that only half the usual number of immune cells will reach the infected area (Kumar et al. 2018). SCI therefore results in reduced ability to fight infection and this means impaired wound healing and increased risk of developing osteomyelitis (bone infection).
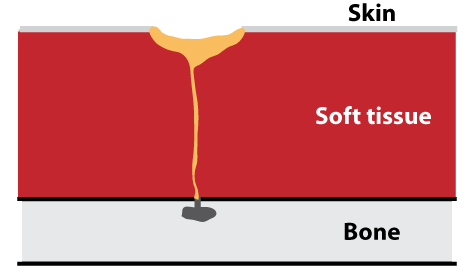
A wound infection that reaches the bone can give rise to osteomyelitis. Once osteomyelitis is present, it will release infective material into the surrounding tissue. This debris is dangerous and the body therefore creates a canal, a draining fistula, to the skin surface through which this material can be removed. The opening of the draining fistula on the skin may look like a wound, but is actually a consequence of the osteomyelitis and it can only be closed by removing the osteomyelitis. Until this happens, it needs to remain open so that the infectious debris can be removed. Osteomyelitis can develop in as little as 2 weeks in worst cases.
Amicapsil can heal the wound, but osteomyelitis can only be removed by surgery and the re-occurrence rate is high. Therefore, don’t wait – treat the wound as soon as it is discovered. The risk of long-term complications are lower, it is quicker, and cheaper.
If osteomyelitis is present, Amicapsil can remove the soft tissue infection. This reduces wound size, the risk of sepsis and improves health status.
New article on Amicapsil-SCI in SCI British Columbia SPIN-magazine
Clinical study with Amicapsil-SCI
Study performed in collaboration with Stoke Mandeville and Salisbury Spinal Injuries Centres (published in Frontiers in Medicine):
- 100% closure rate for acute and chronic wounds and pressure ulcers.
- In wounds resulting from osteomyelitis, i.e. draining fistulas, soft tissue infection was removed. This led to reduced wound size, reduced risk of sepsis, and improved well-being.
- Bed rest not required.
- Treatment was delivered by telemedicine (mobile health). The approach was successful and well received.
Real-world-evidence confirms study
Damian Smith and Mark Ridler from the patient organisation SIA (Spinal Injuries Association) confirmed the findings in an independent survey published in Frontiers in Rehabilitation Sciences:
- 100% closure rate for wounds and pressure ulcers.
- Clinical meaningful improvement of all draining fistulas, e.g. reduced wound size, reductions in autonomic dysreflexia, reduced risk of sepsis, no requirement for bed rest, and improved overall health and QoL.
- Satisfaction with Amicapsil-SCI was: 84% highly positive, 11% positive, 0% negative.
Testimonials


New clinical study with MPPT: 100% closure rate in acute and chronic pressure ulcers
Amicapsil-SCI and acute and chronic wounds, pressure ulcers and burns
Amicapsil-SCI can heal-to-closure close acute and chronic wounds, pressure ulcers and burns in SCI-persons. It is important to start treatment as soon as possible if a wound appears: the sooner treatment starts, the quicker the healing, the less Amicapsil is needed, and the lower the risk of developing osteomyelitis. Therefore, if you have a wound and worry about osteomyelitis start treatment immediately – DO NOT wait for diagnostic tests for osteomyelitis: Osteomyelitis may develop while you are waiting for the test results and none of the existing diagnostic techniques are accurate.
In the clinical trial with Amicapsil-SCI in persons with SCI, the closure rate was 100% for acute and chronic wounds, pressure ulcers and burns, when Amicapsil-SCI was used correctly. These findings were confirmed in an independent survey by the British Spinal Injuries Association. In most of the cases, the individual, family, or carers were responsible for the daily dressing changes with remote support by wound experts to ensure the treatment process was conducted correctly.
Importantly, bed rest is not required.
Osteomyelitis development
Osteomyelitis is infection in the bone. It can develop:
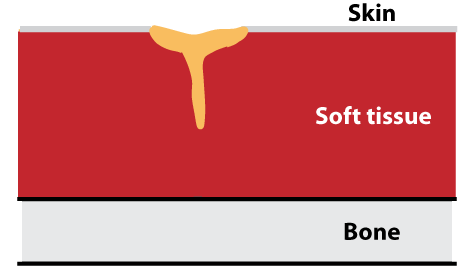
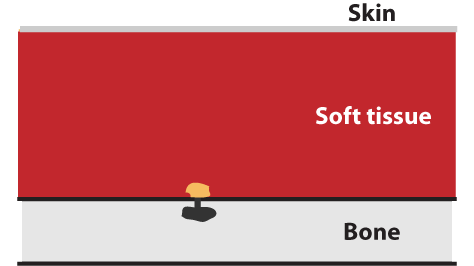
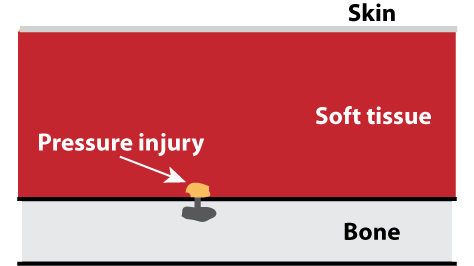
1) from the outside, if an infected wound extends down to the bone and infection enters the bone. A wound is like an iceberg – most of it is below the surface and out-of-sight, which means that you cannot judge how deep the wound is by looking at the surface. A study found that one third of grade 4 wound, i.e. a wound that has reached muscle, give rise to osteomyelitis (Rennert et al. 2009) and that the wound responsible is usually only 4 months old (from first detection) and can be as little as 2 weeks old (Rennert et al. 2009; Russell et al. (2020).
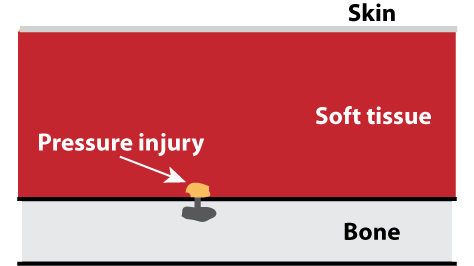
2) from the inside, in two ways:
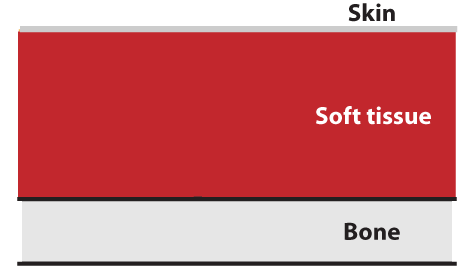
A) if a pressure causes injury to the soft tissue next to the bone, the injured tissue becomes infected, and infection spreads to the bone.
B) If infection spreads via the blood from another area of the body and settles in the bone.
From the outside:
From the inside via pressure (A):
From the inside via the blood (B):
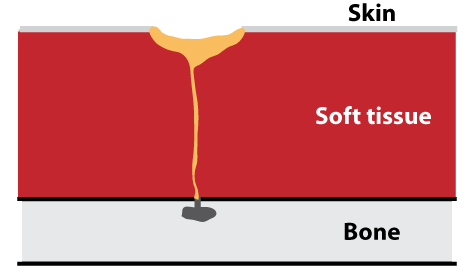
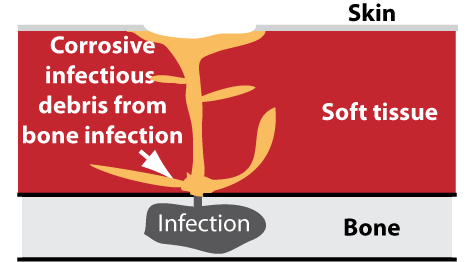
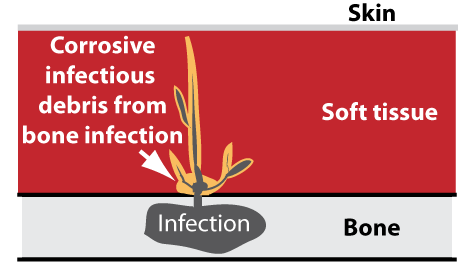
An osteomyelitis will constantly release infectious and corrosive debris into the soft tissue next to the bone. Initially, the body may be able to absorb this debris but after a while, as the volume of debris increases, it will create a canal, a draining fistula, through which the debris can escape to the surface of the body and be disposed of. Consequently, if osteomyelitis develops from the inside, an estuary in the likeness of an ulcer will sooner or later appear on the skin as it discharges (drains) the debris from the infection in the bone through the tunnel (fistula) onto the skin. Such a perceived ulcer will naturally already be extending down to the bone. It is referred to as a draining fistula.
Osteomyelitis and the associated ulcer – the draining fistula
A draining fistula is not a wound, because it is caused by osteomyelitis and it can only close by surgically removing the root cause, i.e. the osteomyelitis (BMJ Best Practice). Because the debris is highly toxic and infectious, a draining fistula often results in a wide-spread festering soft tissue infection causing tissue break-down, malodour, exudate, and a high risk of sepsis.
Osteomyelitis from the outside:
Osteomyelitis from the outside:
Osteomyelitis from the inside:
Osteomyelitis from the inside:
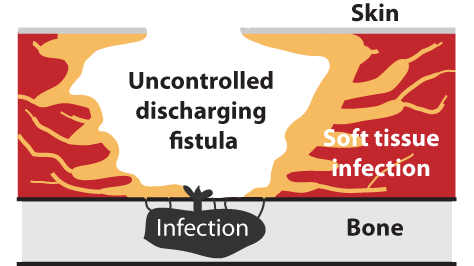
A wound (ulcer) and a draining fistula may look similar, but they are fundamentally different as a wound is damage to the skin and tissue, whereas a draining fistula is a canal through which infectious debris from the bone travels to the skin surface. The draining fistula can only be resolved by removing the infection in the bone. The wound associated with a draining fistula may be closed temporarily via surgery, but will always return if the osteomyelitis is not fully removed. None of the imaging tools currently available are reliably predictive in diagnosing osteomyelitis and even the tool considered the most reliable, i.e. bone biopsy is not fully predictive. Osteomyelitis does usually not show up in blood work and does not necessarily cause fever.
A draining fistula will often look like a wound or a discharging sinus, but it will refuse to close fully with Amicapsil and will often display characteristic signs such as tissue gorges in the wound surface and air bubbles or froth, caused by gas-forming bacteria, appearing in the exudate and on the wound surface. Antibiotics alone are ineffective in treating an osteomyelitis more than 6 weeks old (chronic) (BMJ Best Practice). In chronic osteomyelitis, antibiotics may transiently reduce the level of exudate, but this will frequently increase in volume and/or change in consistency when they are stopped. The antibiotics are likely to make the infection resistant and more aggressive. At the International Spinal Cord Society Conference in Edinburgh, October 2023, Willingsford presented a poster on using markers on the wound surface for diagnosing osteomyelitis.
Chronic osteomyelitis is known for its ability to cause reduced discomfort for long periods of time. However, it can change character quite suddenly, e.g. in connection with a course of antibiotics for a different condition or stress debilitating the immune system for a different reason for a period of time. When that happens, the osteomyelitis can grow quite rapidly and increase the risk of sepsis as well as the infection in the surrounding soft tissue.
The infectious debris from the bone is known to increase the risk of developing cancer in the tissue (Peng et al. 2020).
Russell et al. (2020) reported that the failure rate of surgery at a UK NHS hospital for osteomyelitis was 71% and that two thirds (64%) of the ulcers never healed, even after surgery was repeated. The median time of survival was only 2 years after first surgery if the wound did not heal (64%) and still only 7 years (36%) if it did heal. Panteli and Giannoudis (2017) characterise osteomyelitis as a condition that is managed and not cured.
Osteomyelitis is therefore a condition that is difficult to cure, and it can spread in the body via the blood. This means that preventing a wound from causing osteomyelitis is of utmost importance.
Amicapsil-SCI and osteomyelitis
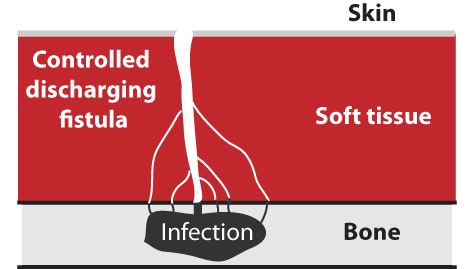
The infection in the bone will constantly grow and release increasing amounts of infectious and corrosive debris into the tissue outside the bone. This leads to a growing draining fistula, which becomes increasingly uncontrollable. In some cases, the body itself is able to create a narrow canal that controls the transport of the debris from the bone to the surface. However, in most cases, the infection and its harmful exudate cause the soft tissue to break down and display an increasingly infected, discharging, malodorous wound that keeps expanding and increasing in severity. This situation increases the risk of sepsis. Amicapsil can help as it removes the soft tissue infection caused by the osteomyelitis and this allows the body to rebuild the tissue and create a stable canal between the bone and the skin surface. Amicapsil will keep the soft tissue lining this path free of infection despite the infectious, corrosive debris passing through it, thereby lowering its harmful impact:
1) This rids the wound of the dead and dying tissue and regenerates new healthy tissue. By doing so, the large uncontrolled wound transforms into a much narrower draining canal.
2) This reduces the risk of sepsis, i.e. blood poisoning.
3) This reduces the level and frequency of autonomic dysreflexia, in particular blood pressure and spasms.
4) Extended bed rest is not needed for Amicapsil to be effective. Bed rest has severe negative impact on both physical and mental health and is incompatible with an active life.
5) Amicapsil is suitable for telemedicine, where the person, family or carers are responsible for the daily dressing changes combined with remote support by a wound expert. This reduces dependence on external nursing visits for dressing changes allowing freedom to perform the dressing change at a time and place that suits one’s own planned schedule and it eliminates waiting.
6) Reducing the size of the wound prior to surgery also reduces the need for or the extend of flap-surgery. The Flap is own tissue taken from a different part of the body and this can have permanent consequences. For example, the buttocks are frequently used, but they are needed for cushioning when sitting, and losing them can complicate sitting after surgery, e.g. making one more prone to future pressure ulcers. Another repercussion is when the donor site refuses to heal.
7) Preliminary evidence indicates that the use of Amicapsil for at least some months before surgery increases the probability of wound closure following surgery substantially.
Depending upon the state of the draining fistula, when starting Amicapsil treatment, it normally takes around 2.5 months to reach a stable state. After this point, the daily amount used will have reduced considerably compared to the beginning of the treatment and will be fairly stable. However, if used very long term, it may slowly increase again as the osteomyelitis itself spreads and generates more debris that causes more harm. Also, long-term, new draining fistulas may develop as the osteomyelitis grows in extent and distance from the original fistula. A new fistula will also require treatment.
What are the official recommendations for treating pressure ulcers?
National Institute for Clinical Excellence (NICE) guidelines recommends:
1) Systemic antibiotics should not be used to treat a pressure ulcer.
2) Topical antiseptics or antimicrobials should not routinely be used to treat a pressure ulcer.
3) NPWT (the pump) is not recommended for routine use on pressure ulcers, except to control the exudate.
4) NICE recommends considering moist wound care (covering the wound with an occlusive dressing). However, for infected wounds this is not an option because the moist environment will exacerbate an infection (https://www.ncbi.nlm.nih.gov/pubmed/28532812).
In conclusion, there are no data to support the use of any of the existing approaches for the treatment of pressure ulcers. This is in line with the recent study by Guest et al. (2018) that only 14% of infected pressure ulcers heal within the first 12 months. The use of antibiotics and antiseptics for other wound types have, in a similar manner, not demonstrated any clinical effects, which led both the FDA and NICE in 2016 to conclude that antibiotics and antiseptics are not effective for treating infected wounds.
Antimicrobials are currently standard-of-care for pressure ulcers, but in the presence of resistant species they will make the infection worse.
