












100% closure rate of pressure ulcers
Download Publication
Download Publication
Download Publication
NH ( patient)
NH ( patient)
NH ( patient)
Only natural ingredients
Only natural ingredients
Only natural ingredients
VH (patient)
VH (patient)
VH (patient)
MPPT - micropore particle technology
MPPT is a novel type of treatment for wounds and dermatological skin lesions. It acts via the wound microbiome to support the immune system, i.e. it is a passive immunotherapy. This means that it acts by enabling the body’s immune system to fight wound infection and regenerate new tissue to close the wound.
MPPT is a Class II medical device and is CE-marked. It is approved as a treatment for wounds, i.e. with a therapeutic claim similar to pharmaceuticals. It has received this approval due to its substantial clinical effects and safety, and it is the only wound product to achieve this.
MPPT is available over-the-counter, i.e. a prescription is not needed. The bottles are not single use. MPPT is temperature sensitive and needs to be stored on refrigeration.
MPPT is available as Amicapsil and Aprobaxil for human use. Amicapsil is approved for all wound types and Amicapsil-SCI for immunocompromised individuals. SertaSil and Adinasil are for veterinary use. Acapsil is a previously used name.
MPPT only involves natural ingredients that are readily biologically recyclable and only water and cotton are used in the process. All packaging is recyclable.

What is infection in a wound or the skin?
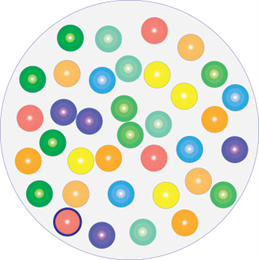
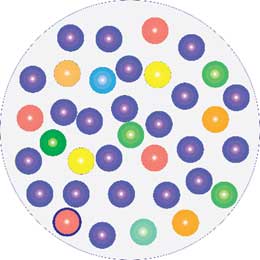
Behind the apparent homeostasis in healthy skin and healing wounds, is a constant microbial back and forth which is under the ultimate control of the immune system. Microbes use two key sets of weaponry, offensive and defensive:
1) they secrete toxins and enzymes to inhibit or kill competing microbes and immune cells;
2) they secrete a shield of biofilm around them, which immune cells cannot penetrate.
Using this weaponry, they take control of the wound.
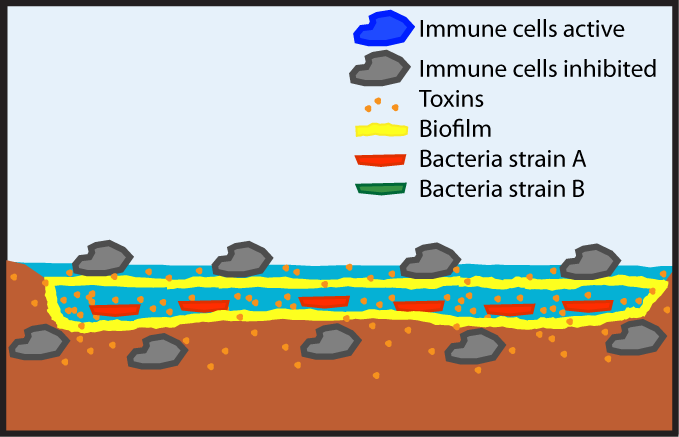
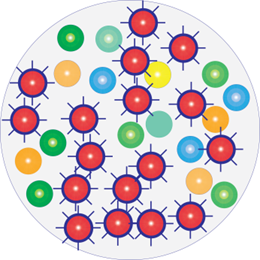
MPPT uses physical forces, i.e. micro-pumping of moisture, to remove the microbial toxins and enzymes and create holes in the biofilm layer. MPPT therefore disrupts the microbes’ weaponry and places the immune system back in control of the wounded area. The immune system can now restore microbial proportion and thereby remove the infection, regenerate tissue and heal the wound. Importantly, it is not MPPT that decides which organisms that should remain, but the immune system.
What does MPPT do?
Behind the apparent homeostasis in healthy skin and healing wounds, is a constant microbial back and forth which is under the ultimate control of the immune system. Microbes use two key sets of weaponry, offensive and defensive, to take control of the wound:
- they secrete toxins and enzymes to inhibit or kill competing microbes and immune cells;
- they secrete a shield of biofilm around them, which immune cells cannot penetrate.
MPPT uses physical forces, i.e. micro-pumping of moisture, to remove the microbial toxins and enzymes and create holes in the biofilm layer. MPPT therefore disrupts the microbes’ weaponry and places the immune system back in control of the wounded area. The immune system can now restore microbial proportion and thereby remove the infection, regenerate tissue and heal the wound. Importantly, it is not MPPT that decides which organisms that should remain, but the immune system.


What happens on the wound?
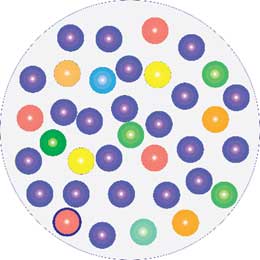
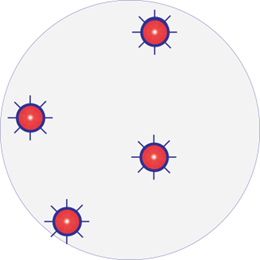
In an infected wound (A), one of a few types of microbes have taken over control by secreting 1) toxins and enzymes to inhibit or kill competing microbes and immune cells and 2) a shield of biofilm, which immune cells cannot penetrate. This prevents the immune system from controlling the wound.
MPPT uses coupled capillary-evaporation, i.e. physical forces, to remove the microbial toxins and enzymes and to create holes in the biofilm layer. The immune cells now regain their functionality and can enter the biofilm fortress, where they can control the microbiome.
Importantly, MPPT does not decide which organisms remain, the immune system does.. In other words, it is each person’s individual immune system that determines what needs to happen.
AMR and wound healing
We all carry antimicrobial resistant (AMR) bacteria. By exposing a wound to antimicrobials, we kill the commensals that help the immune system control the wound environment whilst sparing the resistant organisms. We therefore actively help the resistant strains in taking over control of the wound from the immune system and cause infection (dysbiosis).
Exposing resistant bacterial strains to antimicrobials makes them hypervirulent, i.e. hyper-aggressive. Since we have now put them in control, they will infiltrate even more aggressively than before and aggravate the wound.
Studies have shown that antibiotics delay wound healing. Also, both antibiotics and antiseptics contribute to AMR, including cross-resistance.
US FDA on existing treatments
FDA (2016): Classification of Wound Dressings Combined with Drugs
“The available evidence does not appear to demonstrate improved clinical outcomes from the use of antimicrobial dressings over non-antimicrobial dressings for the prevention or treatment of local wound infections or to improve wound healing.”
FDA (2022): Advancing product development for non-healing chronic wounds.
“Despite the public health burden, innovative products aimed at the treatment of non-healing chronic wounds are lacking.”
“innovative product development is essential to addressing the unmet medical need of non-healing chronic wounds”.
Clinical effects of MPPT
Clinical trial in pressure ulcers in spinal cord injured (SCI)
MPPT resulted in 100% closure rate of acute and chronic wounds and pressure ulcers. All the chronic wounds had, prior to MPPT, been treated unsuccessfully with antimicrobials.
MPPT controlled soft tissue infection caused by an underlying osteomyelitis. This reduced wound size and risk of sepsis.

Wounds, ulcers and burns
Amicapsil for humans
Trauma and surgical wounds, pressure ulcers, venous leg ulcers, diabetic foot ulcers, burns, etc.
SertaSil for animals
Trauma and surgical wounds, abscesses, amputations, and burns in dogs, horses and other animals.
Dermatology
Aprobaxil for humans
Acne, pyoderma gangrenosum, hidradenitis suppurativa, atopic dermatitis, zits etc
Adinasil for animals
Eczema, dermatitis, lick granuloma, insect bites, autoimmune skin conditions, etc.
Evidence
Effects of SertaSil on wound healing in the rat.
A preclinical study (Bilyayeva et al., 2014) was performed in a rat wound healing model, comparing MPPT to topical gentamicin and untreated controls. An aseptic wound was induced by administering 1ml 10% calcium chloride solution into the subcutaneous layer under local anaesthesia. Following opening of the abscess, animals were divided into a control group (no treatment) and either MPPT (SertaSil) or gentamicin, which were applied topically to the wound every 24 hours until a non-infected wound was achieved, i.e. free from necrosis, pus and fibrinogenous thickenings.
Rats (n=15 per group) receiving MPPT reached the non-infected wound stage in 3.0±0.4 days (mean±SD) compared to 7.0±0.4 days for gentamicin and 10.0±0.4 days for control. Time to wound closure was 13.9±0.3 days for MPPT, 18.7±0.6 days for gentamicin, and 23.0±0.4 days for control. The surface area of the wounds was measured at day 1 and day 13. At day 1, the wound surface areas (mm2) were similar in all three groups (157.4±8.9), but at day 13 the MPPT group had significantly smaller wound areas (5.2±1.7) compared to the gentamicin (38.0±1.5) and control groups (95.7±11.3).
The study was conducted in young rats that were still growing and gaining weight. At day 19, only the rats receiving MPPT exhibited a weight increase (271±5g) indicating good recovery, whereas rats receiving gentamicin did not gain weight (249±5g) and rats in the control group lost weight (242±16 g).
The MPPT group demonstrated a significant and considerable increase in number of immune cells migrating to the wound relative to the comparators. Compared to the topical antibiotic gentamicin, the MPPT group after 48 hours had a 107% (2.1-fold) increase in the overall number of immune cells in the wound, including a 24.8-fold increase in the number of macrophages and a 7.2-fold increase in lymphocytes; the levels of immune cells were similar in the gentamicin and untreated control groups. Wound bacterial colonisation was similar in the MPPT and untreated control groups, demonstrating that MPPT is not antimicrobial. As expected, gentamicin reduced the number of bacteria. No adverse events were seen.
Comparative Clinical Study of the Wound Healing Effects of a Novel Micropore Particle Technology: Effects on Wounds, Venous Leg Ulcers, and Diabetic Foot Ulcers.
The safety and efficacy of MPPT for treating wound infections were evaluated in a 266 patient in-hospital randomized, comparative clinical trial (Bilyayeva et al., 2017). The study compared MPPT to topical gentamicin (antibiotic) and topical iodine (antiseptic). The study included patients with primarily trophic ulcers caused by pancreatic diabetes and venous insufficiency of the lower extremities, abscesses including carbuncles and furuncles, phlegmons, infected third- or fourth-degree burns, and infiltrations of postoperative wounds. The products were applied topically to the wounds once daily until they were free from necrosis, pus, and fibrinogenous thickenings.
The number of days (mean ± standard deviation) to removal of wound infection was 3.0 ± 0.9 for MPPT (n = 88) compared with 7.0 ± 1.2 and 8.0 ± 1.1 for gentamicin (n = 90) and iodine (n = 88), respectively. Thus, MPPT reduced the time to reaching a non-infected wound by 57% and 62%, respectively. The products were used once daily until a non-infected wound was reached, and number of days therefore also reflects the number of applications. Days to onset of granulation for MPPT, gentamicin, and iodine were 4.5 ± 0.8, 9.2 ± 1.4, and 10.3 ± 1.5 days, respectively; and days to onset of epithelialization were 7.8 ± 1.1, 14.1 ± 1.9, and 16.4 ± 2.7 days, respectively. Subgroup analysis of patients with diabetic foot and venous leg ulcers found that each of these demonstrated the same pattern of infection removal and healing as the overall study.
The number of hospitalization days was 14.6 ± 5.6 for MPPT, 21.0 ± 10.7 for gentamicin, and 24.0 ± 7.9 for iodine. Compared with gentamicin, patients receiving MPPT had a 31% reduction in hospitalization duration and a 39% reduction compared with iodine. In the subgroups, MPPT reduced the number of hospitalization days compared to gentamicin by 41% for acute wounds; 31% for diabetic foot ulcers; and 19% for venous leg ulcers and, compared to iodine, by 44% for acute wounds; 51% for diabetic foot ulcers; and 36% for venous leg ulcers. No adverse events were reported, except for a transient increase in pain-levels in some venous leg ulcers, which appears to be related to this specific condition.
In this clinical study and in the preclinical study, the effects of MPPT and gentamicin on time to reaching a non-infected wound were the same. This supports the validity of the findings and that MPPT is more effective than antibiotics and antiseptics in achieving a non-infected wound.
Clinical evaluation at Bristol University Hospital
Prospective case-series (Ryan, 2017) at Bristol University Hospital, covering nine acute dehisced surgical wounds and one category 4 pressure ulcer (non-SCI). Standard-of-care in the hospital was 1 week with UrgoClean followed by 2 or more weeks with NPWT until reaching a healing wound; where possible the patient would at this stage be discharged into community care.
Wounds receiving MPPT reached this infection-free healing stage in 3-5 days and all wounds that could be followed proceeded to full closure without complications. No adverse events reported.
The time to reach a non-infected and healing wound in this study are the same as in the pre-clinical study in rats and the RCT, and this confirms the validity of the findings and the effects of MPPT.
Time to Abandon Antimicrobial Approaches in Wound Healing: A Paradigm Shift.
Review article (Sams-Dodd and Sams-Dodd, 2018) presenting evidence on the mode-of-action of MPPT and a review of clinical evidence, including new case-reports.Micropore Particle Technology Promotes Wound Healing, Whereas Polyhexamethylene Biguanide Causes Tissue Degeneration: A Case Report.
Case-report of 72-year-old woman with a nontraumatic spinal cord injury, who developed eschar on her lower right back (Sams-Dodd and Sams-Dodd, 2020). An underlying abscess was identified, which upon surgical debridement left a large wound extending down to the hip bone. In addition, the hip suffered from chronic osteomyelitis and was exposed at the bottom of the wound constituting 25% of the wound bed. The wound was 12 cm x 3 cm and 6 cm deep. There was severe undermining measuring 2 cm to 4 cm in depth along half of the perimeter of the wound. A 20 cm deep and 3 cm wide tunnel exited from the bottom of the wound down along the right femur, which also suffered from chronic osteomyelitis.
The wound was initially treated for 5 weeks with Manuka honey but deteriorated further. Next, micropore particle technology (MPPT) was used. It cleared the wound, including the tunnel, of necrotic tissue based on autolytic debridement and removed the soft tissue infection; over a 3-month period, the wound reduced 50% in volume.
The treatment approach was changed to polyhexamethylene biguanide (Prontosan), which was applied as a gel once every second day to the wound. After 6 days, it was observed to cause tissue degeneration, disruption of the structure of the exposed bone, and the appearance of froth coming from the disrupted hip bone. A pain syndrome developed and the use of PHMB was terminated on Day 10. After a wash-out period, the use of MPPT was reinitiated.
Over the following 8 months, MPPT continued to control the infectious debris coming from the hip bone and promote healing without affecting the bone or causing side effects. It is generally assumed that the cytotoxic properties of antiseptics seen in cell culture experiments do not occur on wounds.
The present case is consistent with the antiseptic PHMB being released into the wound and with its cytotoxic properties being expressed and leading to disruption of tissues and tissue regeneration.
Novel micropore particle technology for spinal cord injury chronic wound healing: a new paradigm?
Case-report by the Defence Medical Rehabilitation Centre (Ministry of Defence) on the use of MPPT for treating a 7 month old abscess in a person with spinal cord injury (SCI) (O’Sullivan et al., 2020). Several treatments, including surgery twice, had unsuccessfully been tried and the wound was deteriorating. The authors’ write:
- “The chronicity of the wound, especially the smell, impacted negatively on the psychological well-being and physical rehabilitation of the patient. He required increased bed rest, reducing his time in the wheelchair, and leading to a dramatic loss of independence.“
- “After the first 4 weeks [with MPPT], there was a dramatic improvement in the wound with dimensions and exudate levels substantially reduced and epithelisation visible. Within a week of starting, the wound odour had disappeared.”
- “After 3 months, there was a minimal residual open area to the wound with a very low exudate level, and by 6 months, full resolution of the wound was nearly reached with the wound in the remodelling stage. The patient encountered no adverse effects as a result of his MPPT therapy.”
- “This patient had a chronic wound, unresponsive to traditional treatment for 7 months. After 1 month of MPPT, significant improvement was noted, with resolution after 6 months. It has empowered the patient to have increased involvement in his care and fully engage in his overall rehabilitation potential.”
- “MPPT has the potential to improve the management of chronic wounds at DMRC with its ability to heal wounds quicker. Patients undergoing rehabilitation will be able to engage fully sooner, with earlier intervention reducing the need for surgical interventions, secondary complications, treatment duration, cost and improve patient quality of life and effective rehabilitation.”
Pyoderma gangrenosum ulcers treated with novel micropore particle technology
Prospective case-series by Birmingham University Hospitals, using MPPT for treating 3 cases of pyoderma gangrenosum (Lovgren et al., 2018). Participants were followed for a 3-month-period and, in all cases, MPPT induced a healing process that continued throughout the observation period. In one of the patients, it was possible to reduce the dose of immunosuppressants. In an additional unpublished case, MPPT was used in one pyoderma gangrenosum-patient with an active, resistant infection precluding the use of immunosuppressants. MPPT was, after once daily application for 5 days, able to remove the infection and to promote healing.
Stable closure of acute and chronic wounds and pressure ulcers and control of draining fistulas from osteomyelitis in persons with spinal cord injury: non-interventional study of MPPT passive immunotherapy delivered via telemedicine in community care (Sams-Dodd et al., 2024).
- Persons with spinal cord injury (SCI) are immunocompromised due to the loss of connection between the immune and the nervous systems and display strongly impaired wound healing. There is no recognised treatment approach for pressure ulcers in SCI-persons and an ulcer can rapidly cause osteomyelitis and sepsis. ICH E10-guidance (ICH 2000) instructs comparators cannot be included in a study if this may expose participants to risk of irreversible morbidity or death. MPPT had previously demonstrated efficacy on infected wounds and the study was therefore single-arm.
- The study included 44 wounds and pressure ulcers. It was performed in collaboration with the two main UK spinal cord injury centres, Stoke Mandeville (National Centre) and Salisbury.
- Treatment was delivered using a telemedicine approach. Patients, family or carers were responsible for hands-on dressing changes, and they would daily send pictures of the wound to a wound specialist and would, before next dressing change, receive advice on how to proceed the following day, i.e. if any changes in procedure were recommended.
- All (100%) acute and chronic wounds and pressure ulcers treated with MPPT reached full and stable closure. All chronic wounds had been treated with antimicrobials unsuccessfully prior to MPPT. Some acute wounds had also been exposed to antimicrobials before MPPT. Prior exposure to antimicrobials appeared to impede healing.
- If osteomyelitis is present, a draining fistula (canal) between the bone and the skin will always develop to allow infective debris generated in the bone to escape. Frequently, this fistula progresses into a large festering uncontrolled wound that increases the risk of sepsis. MPPT was able to control the infection in the soft tissue caused by the bone debris and to reduce the fistula to a controlled narrow canal without soft tissue infection, thereby reducing the risk of sepsis until surgery. (Chronic osteomyelitis, i.e. more than 6 weeks old, can only be resolved surgically.)
- Normally SCI-persons with a non-healing wound are placed on extended bed rest – sometimes for years. Bed-rest is not a requirement for MPPT, meaning that people can have an active lifestyle. This avoids the many follow-on conditions from extended bedrest and inactivity.
- No adverse events or side-effects were observed or reported. MPPT was used daily on the same area by 11 participants for more than 6 months and of these by 5 patients for more than 12 months; the latter included direct daily application onto bone with chronic osteomyelitis and one participant was on anticoagulant therapy. No adverse effects on skin, muscle, tendon and bone were observed and MPPT was not, including in hyperallergic participants, associated with any allergies, irritation, bleeding etc.
- MPPT would provide cost-savings in the order of 74% to 89% per wound the first year alone and 100% the subsequent years because the wounds close.
- The study demonstrated that MPPT is safe and effective in immunocompromised persons.
Patient-reported outcome survey of user-experiences in the spinal cord injured-community with MPPT for treating wounds and pressure injuries and for controlling soft tissue infection caused by osteomyelitis. Authors: Damian Smith and Mark Ridler, Spinal Injuries Association, UK
Background:
People with spinal cord injury (SCI) are at high risk of developing pressure injuries. Reports in the SCI-community had indicated that a new class of wound treatment, MPPT (micropore-particle-technology), was effective in treating pressure injuries. The British Spinal Injuries Association therefore conducted a survey among MPPT-users to learn from their experiences.
Methods:
Online survey restricted to individuals with spinal cord injury. Participants were requested to identify themselves to permit validation of statement.
Results:
The survey had 41 respondents reporting on a total of 49 wounds of which the two main categories were wounds (n = 33), primarily pelvic pressure ulcers; and draining fistulas (n = 9) caused by osteomyelitis. All wounds reported had reached full closure. Median duration of MPPT use and time to closure were 3 and 4 weeks for acute wounds (<6 weeks old) and 8 and 10 weeks for chronic wounds, respectively. On draining fistulas, MPPT had been used to reduce wound size, remove soft tissue infection, avoid sepsis, reduce autonomic dysreflexia, improve overall health, and avoid bed rest, whilst waiting for surgery. Comments on MPPT were 84% highly positive, 11% positive, and 0% negative. No adverse events were reported.
Conclusions:
MPPT achieved a 100% closure rate of acute and chronic wounds, and, in draining fistulas, effectively controlled soft tissue infection resulting from osteomyelitis. MPPT does not require bed rest and is suitable for self-care and telemedicine, promoting independence and higher quality-of-life. The findings strongly agree with a recent clinical study of MPPT.
Medical and scientific conferences









Publications and Abstracts
- Smith, D. and Ridler, M. (2024) Patient-reported outcome survey of user-experiences in the spinal cord injured-community with MPPT for treating wounds and pressure injuries and for controlling soft tissue infection caused by osteomyelitis. Frontiers in Rehabilitation Sciences
- Sams-Dodd, J., Belci, M., Bandi, S., Smith, D., and Sams-Dodd, F. (2024) Stable closure of acute and chronic wounds and pressure ulcers and control of draining fistulas from osteomyelitis in persons with spinal cord injury: non-interventional study of MPPT passive immunotherapy delivered via telemedicine in community care. Frontiers in Medicine
- Smith, D (2023) Addressing the challenges of treating pressure ulcers following spinal cord injury with Amicapsil-SCI micropore particle technology.ISCoS, Edinburgh, 8’th to 11’nd October, abstract #56. See Abstract and Poster
- Sams-Dodd, F. and Sams-Dodd, J. (2023) MPPT for controlling soft tissue infection caused by osteomyelitis. ISCoS, Edinburgh, 8’th to 11’nd October, abstract #98.
- Sams-Dodd, F. and Sams-Dodd, J. (2023) Diagnosing osteomyelitis using wound characteristics and response to MPPT. ISCoS, Edinburgh, 8’th to 11’nd October, abstract #187.
- Sams-Dodd F. and Sams-Dodd, J. (2023) Effective treatment of wound infections using physical interactions with the microbiome – without the use of antimicrobials. Online symposium May 22-23, 2023, University of Gibraltar.
- Sams-Dodd, F. and Sams-Dodd, J. (2023) Evaluating a passive immunotherapy acting via the microbiome for treating injured and infected dog tails: a prospective case-series. BSAVA, Manchester, March 23-25.
- Sams-Dodd, F., Belci, M., Smith, D. and Sams-Dodd, J. (2022) MPPT, delivered by a telemedicine approach, for treating acute and chronic wounds and pressure ulcers in SCI-persons. ISCoS, Vancouver September 15-18, abstract #295.
- Sams-Dodd, F. and Sams-Dodd, J. (2022) Effective Treatment of Burn Infections by Supporting the Immune System and the Microbiome. MHSRS, September 12-16, Orlando, Fl. USA, abstract MHSRS-22-05489.
- Sams-Dodd, F. and Sams-Dodd, J. (2022) Antimicrobial Development to Counter Wound Infections in Military Personnel. MHSRS, September 12-16, Orlando, Fl. USA, abstract MHSRS-22-05487.
- Sams-Dodd, J., Belci, M., Bandi, S., Smith, D. and Sams-Dodd, F. (2021) Micropore particle technology – new treatment for wounds and pressure ulcers in SCI-persons. ANZSCoS, October 27-29, 2021, Session 3A.
- Sams-Dodd, J., Belci, M., Bandi, S., Smith, D. and Sams-Dodd, F. (2021) Micropore particle technology – new treatment for wounds and pressure ulcers in SCI-persons. EPUAP, September 14-16, Abstract FPS3.1
- O’Sullivan O, Hayton L, Findlay-Cooper K, Phillip R. Novel micropore particle technology for spinal cord injury chronic wound healing: a new paradigm? BMJ Mil Health. 2020 Aug 4. Epub ahead of print.
- Sams-Dodd J and Sams-Dodd F. (2020) Micropore Particle Technology Promotes Wound Healing, Whereas Polyhexamethylene Biguanide Causes Tissue Degeneration: A Case Report. Wounds 32(3):E6–E10.
- Sams-Dodd, F. and Sams-Dodd, J. (2019) Micropore particle technology effectively treats infected wounds and pressure injuries in patients with spinal cord injury. ISCoS, Nice Nov. 5-7, 2019.
- Sams-Dodd J and Sams-Dodd F. (2018) Time to Abandon Antimicrobial Approaches in Wound Healing: A Paradigm Shift. Wounds 30(11):345–352.
- Lovgren ML, Wernham A, James M, Martin-Clavijo A. Pyoderma gangrenosum ulcers treated with novel micropore particle technology. Br J Dermatol. 179(Suppl 1):BI22, 152.
- Ryan E (2017) The use of a micropore particle technology in the treatment of acute wounds. Journal of Wound Care 26(7): 404-413.
- Ebony Ryan, Bristol University Hospital:
Clinical evaluation of a novel MMP wound care product on wounds to heal by secondary intervention. TVS 2017 – The Conference, Poster no. 1. - Sams-Dodd, J. and Sams-Dodd, F. (2017) MPP inactivation of bacterial defences: 60% reduction of inflammatory phase and faster healing. TVS 2017 – The Conference, Poster no. 3.
- Bilyayeva O, Neshta VV, Golub A, Sams-Dodd F. (2017) Comparative Clinical Study of the Wound Healing Effects of a Novel Micropore Particle Technology: Effects on Wounds, Venous Leg Ulcers, and Diabetic Foot Ulcers. Wounds Epub 2017 May 25.
- Bilyayeva O, Neshta VV, Golub A, Sams-Dodd F. (2014) Effects of SertaSil on wound healing in the rat. J Wound Care. 23(8):410, 412-4, 415-6.
- Bilyayeva, O.O; Neshta, V.V., Golub, A.A; Sams-Dodd, F. (2011) Promotion of wound cleansing and acceleration of healing by antimicrobial sorption. EWMA May 23-25, 2011. Abstract P42.
