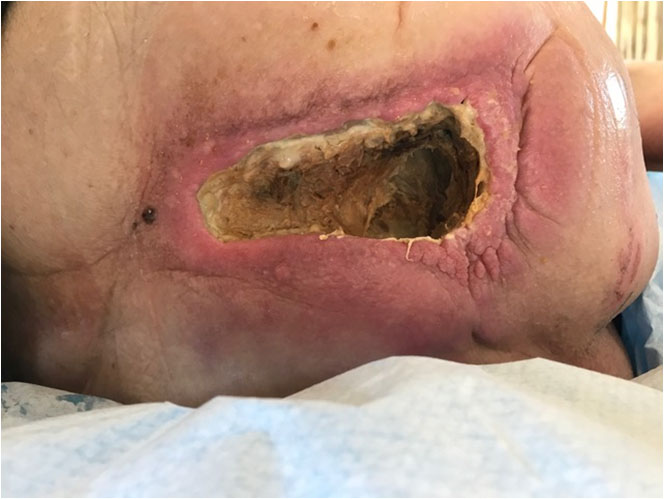
A 74-year-old lady had received very high doses of radiotherapy 35 years ago to treat cervical cancer. This had created an abscess which 35 years later, in March 2017, revealed itself as a sizeable patch of eschar (dry, black necrosis) on the right side of the lower back (Pict. 5 April 2017, see below).
Approximately a month and a half later (Pict. 20 May 2017), the patient developed toxaemia; was hospitalised to ICU (intensive care unit); and received iv antibiotics for 4 days where-after the abscess was surgically debrided, exposing an infected wound with a 10 x 2.5 cm opening. The depth was 6.5 cm without finding viable tissue at the bottom. The “floor” of the wound, as it appears in the pictures, was directly on top of bone suffering from chronic osteomyelitis. This bone infection needed to drain into the wound.
 |
 |
| 5 April 2017 | 20 May 2017 – Day before surgical debridement |
For one month following this debridement, the wound was packed daily with Manuka honey and dressed with superabsorbents to resolve the remaining necrotic tissue and to promote healing. However, after a brief appearance of a few granulation buds at one edge (Pict. 13 June 2017), the wound regressed, grew in size to 12×3 cm and the necrotic tissue dried and formed a 1 cm thick dry and leathery layer on top of the entire wound. A severe, deep and wide undermining along half the perimeter of the wound developed and the skin significantly thickened and hardened (an indication of the potential presence of toxins). Broad purple-red wound edges and peri-wound area were evident, indicating high risk of cellulitis. The wound became increasingly infected and highly malodorous and the patient showed overall renewed signs of toxaemia (Pict. 23 June 2017).
 |
 |
| 13 June 2017 – after 3 weeks with Manuka honey | 23 June 2017 – Day -4 – four days before start of Amicapsil |
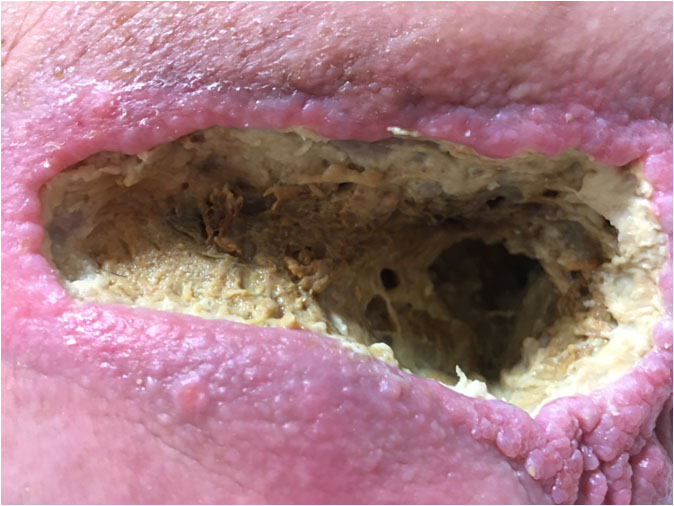
On the 27th of June, Day 0, the use of Manuka honey was stopped and daily application of Amicapsil was initiated. A MRI was performed, which identified a 20 cm deep 3 cm diameter tunnel, leading from the right-side bottom of the wound down along the right femur. This was running along the main vessels and nerves and was tightly filled with cheese-like slough. Similar to the hip-bone, the femur also suffered from chronic osteomyelitis and needed to drain into the tunnel. The wound was washed and Amicapsil applied. After 24 hours, the overall signs of toxaemia had reduced (not disappeared) and the wound showed signs of granulation to the front rim at the leftmost corner, the “ceiling” and the “floor”(Pict. 28 June 2017, Day1).
 |
 |
| 28 June 2017 – Day 1 – After 24 hours Amicapsil | 5 July 2017 – Day 9 |
Over the following months, with some interruptions, the wound was thoroughly washed and Amicapsil was applied more or less daily to roughly all accessible wound surfaces, including exposed osteomyelitic bone, undermining and as far possible into the tunnel until blocked by slough. It was covered with a permeable contact layer dressing and a 2-ply gauze.
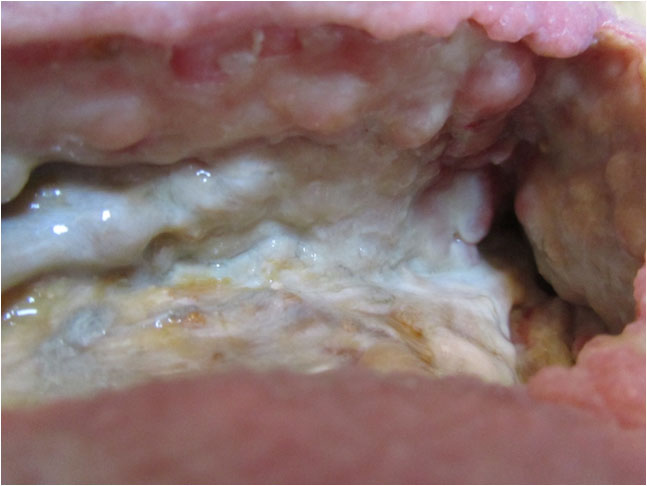
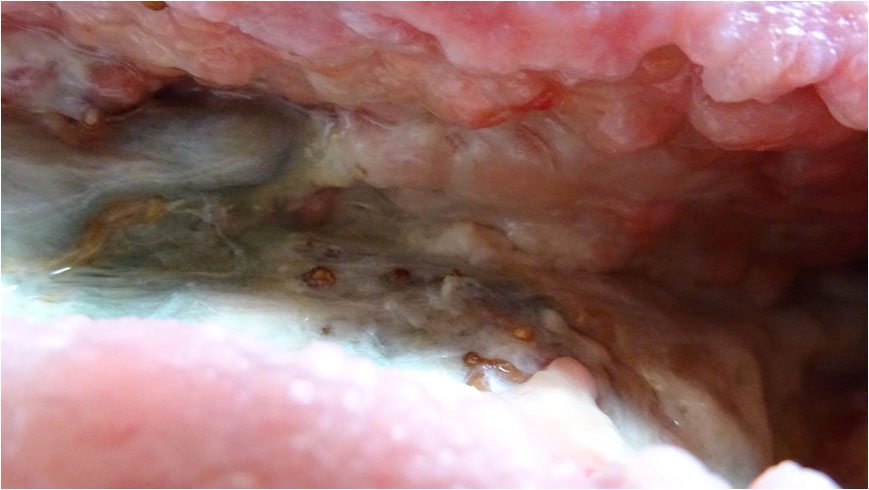
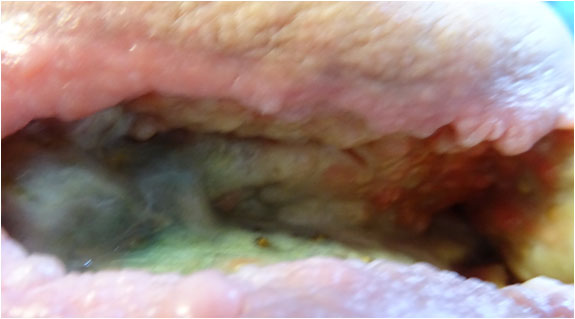
The wound progressively cleared and granulation tissue and new epithelium around the wound edges appeared and grew gradually stronger (Pict 05 July 2017, Day 9). The malodorous infection of the entire wound resolved. The ongoing necrotizing stopped, large amounts of the existing necrosis dissolved via autolysis and the underlying viable tissue started to build up via steady granulation. (Pict. 23 July 2017). In the floor-area of the right hand side of the wound in front of the hole marking the entrance to the 20 cm deep sinus, an area gradually cleared very deep down until reaching viable tissue, including a 0.5 cm wide, 10 cm long and 4.5 cm deep ridge (Pict. 25 July 2017).
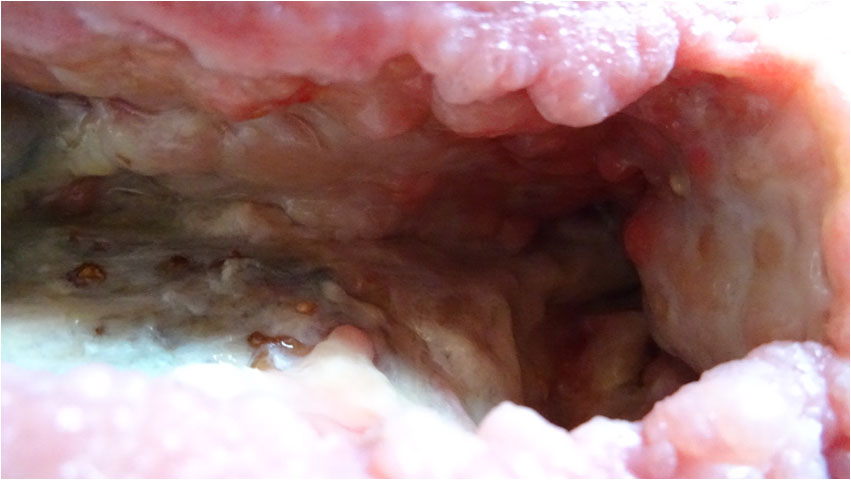
The left hand side of the floor area was situated on top of the osteomyelitic bone. This was cleared of the necrotic tissue whilst still preserving the white structured fascia on top of the bone. The chronic infection had deformed the bone structure to the degree that it was no longer smooth but butting up grey and brown protrusions through the fascia. Granulation started to grow back over the bone where the fascia was intact. (Pict. 25 July 2017)
 |
 |
| 23 July 2017 | 25 July 2017 |
 |
| 30 July 2017 – The area between the granulating “ceiling” and the white and structured fascia on the “floor” is a necrotized vein that is in undergoing removal by autolytic debridement. |
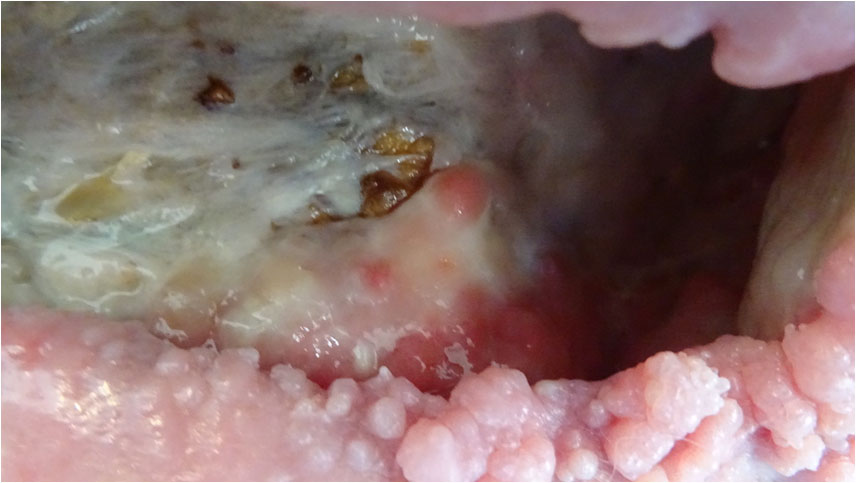
During the course of the following month, the wound would build strong new tissue from the entire ceiling and right-hand side of the wound (Pict. 02 August 2017) (Pict. 17 August 2017) as well as the right-hand side deep floor area in front of the sinus entrance (Pict. 29 August 2017 – 1). For reasons external to Amicapsil and the wound, the left upper corner had up till now mostly been left uncovered with Amicapsil during applications and was, therefore, lacking behind still needing to undergo autolytic debridement of necrotized non-soft-tissue, e.g. vessels (Pict. 29 August 2017 – 2).
 |
 |
| 2 August 2017 | 17 August 2017 |
 |
 |
| 29 August 2017 – 1 | 29 August 2017 – 2 |
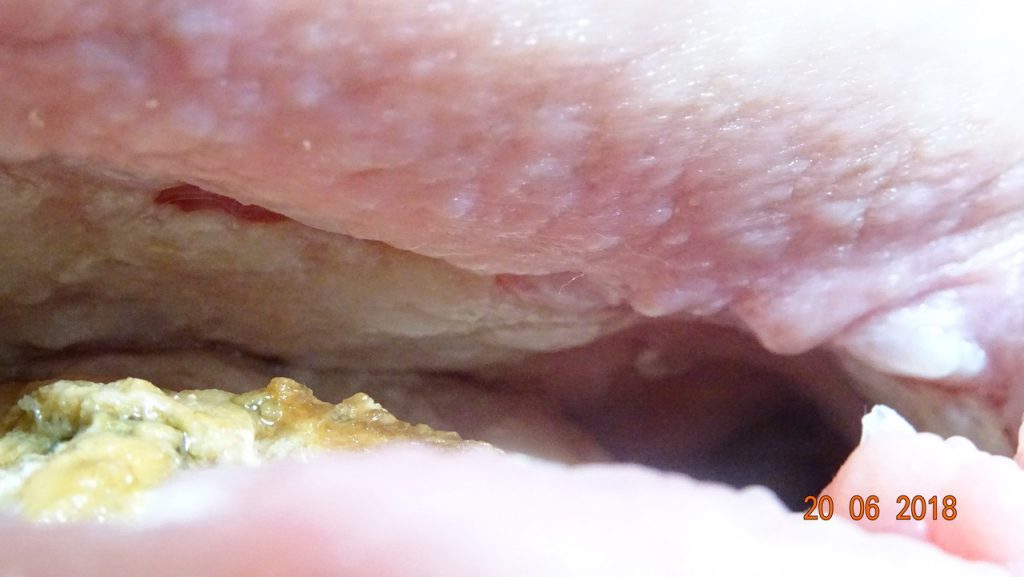
After 2 months with Amicapsil, 31 August 2017, the 20 cm deep sinus down the leg running along the osteomyelitic bone cleared of the remaining cheese-like slough and remained clean. Only one day later, there was a remarkable change in the purple-red coloured cellulitic peri-wound skin. The inflammation started to contract in width and the skin gained a healthy pink colour. At this point in time, the hardened skin along the entire bottom edge of the wound also started to slowly fuse at the bottom thereby starting to clear the undermining. Further, off-white coloured new epithelium generated on the edges themselves. Furthermore, the volume of the wound had reduced considerably (Pict. 02 September 2017).
 |
| 2 September 2017 |
The high-risk issues in the wound had been resolved, the healing was progressing well, and it was decided to change the application regime to every other day.
The wound continued to move rapidly along the path of healing with granulations building from the ceiling; back wall; right hand side of wound; and floor area in front of the right hand sinus entrance (Pict. 13 September 2017) (Pict. 07 October 2017). The osteomyelitic left-hand side floor area was kept clean and granulation was slowly making its way over the fascia (Pict. 13 September 2017) (Pict. 17 October 2017 -1).
By mid October, the wound had reduced approximately 50% in volume (Pict. 17 July 2017-2); there were no signs of wound infection; and the patient was overall performing remarkably well.
 |
 |
| 13 September 2017 | 7 October 2017 |
 |
 |
| 17 October 2017 – 1 | 17 October 2017 – 2 |
General observation:
For the duration of the period of Amicapsil use, a consistent feature was that as soon as an area had been cleared of necrosis, it started to granulate. Granulation would always make its first appearance as a distinctive white layer of proliferating cells and over the following couple of days, this would turn pink as the angiogenesis took place and the granulation matured.
Another consistent trait throughout the period of removal of infection and necrotic tissue as well as tissue formation was, that the immune system would seem to work the deeper tissue and deposit the resulting waste as sloughy exudate on top of the wound, even on top of areas with strong granulation. The healing process was, therefore, assisted by a daily wash to remove this toxin containing waste material without causing damage to the forming granulation tissue.
The wound as a small part of a bigger clinical picture – Amicapsil used for tertiary intention healing:
Due to the presence of extensive and chronic osteomyelitis (bone infection), the patient had been referred to the national specialist unit for osteomyelitis at Nuffield in Oxford. Osteomyelitis of this magnitude, severity and in the relevant area could only be treated via life-threatening major surgery and with uncertain future perspectives of quality of life for the patient. The consensus of the specialist team was, therefore, to try to manage – not cure – the osteomyelitis with the use of antibiotics. The success of this option would, however, depend on this extensive and infected body opening (the wound) being brought under control. Furthermore, as the infection of the bone would persist, it would always continue to drain microbes and their toxins into the wound. Therefore, a long-term solution to manage these conditions and avoid further infection or necrosis in the wound was sought for.
The wish-list for the wound set out by the specialist team in Oxford was to:
- remove all dead tissue and waste material originating from the infection (debride) as this is the ideal breeding ground for infections;
- remove the wound infection;
- maintain the wound clean without it growing in size or complexity; and
- keep infection and amount of toxins in the wound below the threshold of causing toxaemia.
At this point in time, Amicapsil had accomplished all of these wishes and was continuing to keep the wound controlled and healing. All expectations had, consequently, been exceeded and the patient could go back to the team in Oxford with high hopes.
The patient and her family offered the following statement:
Testimonial for Amicapsil.
21st October, 2017.
For the period from March 2017/October 2017.
TESTIMONIAL
35 years ago my wife was one of the first people to live through cervical cancer after having been given a few months to live. She was at Christies Hospital in Manchester and given a new treatment which included a very heavy dose of radiotherapy.
Seven months ago, this long forgotten radio-therapy resurfaced by creating various abscesses in her pelvis and thigh. When the surgeons opened up what seemed to be a large pressure sore, they were amazed to find a deep wound created by escaping radiotherapy infection from her pelvis and thigh. What they found was a rectangular wound that was 12 cms wide, 5 cms deep and 12 cms into her flesh at it’s deepest point which fed into a 20 cm sinus that ran into the bone. They decided it was too dangerous to continue clearing it and referred us back to the deep tissue viability team.
After a further two months, with the use of traditional methods there was little improvement and we firmly believed that my wife would die as the infection worsened. Nobody gave us any assurances that this was not the case. All they knew was that she had chronic osteomyelitis which seemed incurable without a deep tissue operation at the Nuffield Centre, which had less than a 50% chance of survival.
We were then introduced to a product called Amicapsil. The manufacturer, at that time, thought the wound was too severe for its product to work, but we decided to take a chance. Nothing else was working. Within a month there had been a major improvement. Now, just after two months the wound and the sinus are almost totally clear; granulations are blooming and the flesh has closed down the wound by approximately 50%. Unbelievable. We have kept an accurate photographic record, always with community nurses present, of this amazing transformation.
The surgeons and doctors had said they couldn’t do anything with the wound in the condition it was in. We’re now going back to them with an almost clean wound. My wife is in little pain and full of hope as we wait to see what the surgeons and doctors now determine how they can prolong her life.
We’re not home yet, but without Amicapsil neither of us believes we would have got this far.
JS and ES
The wound was taken off Amicapsil treatment and the plan was to return to the original team in Oxford with a non-infected, granulating wound on top of osteomyelitic bone. Unfortunately, external circumstances prevented this re-evaluation of the wound and the patient’s clinical possibilities. After a short period off Amicapsil, the wound started to break down due to the use of an antiseptic (see the case here). She was, consequently, put back on Amicapsil treatment again in November 2017. During the following months, the wound continued to reduce in size whilst the Amicapsil kept the adjacent infection at bay.

The patient now engaged with a consultant surgeon at the Royal National Orthopaedic Hospital who evaluated the wound itself and the soft tissue in the entire area, i.e. down along the femur, the entire right buttock region and the area along the spine. He judged the degree of infection, (tissue infiltration) to be sufficiently small and controlled, to make possible the surgical removal of the infected entire hip-bone, followed by closure of the wound. This procedure was performed in stages during October-November 2018. See picture below from 15th Oct.
Amicapsil is indicated also post-surgery, to ensure the graft takes and to prevent infection in the deeper areas.
Due to the extent of the surgical procedure, it was necessary to permit for a short period of rest before, the final plastic follow up with flap operation. This was performed in December 2018 and the patient arrived home in time for Christmas.














